Ideally, all women would have excellent experiences with family planning care. But according to a Child Trends analysis of new data from the 2017-2019 National Survey of Family Growth (NSFG), less than three quarters of all women rated their experiences with their family planning provider as “excellent” (versus “very good,” “good,” “fair,” or “poor”), across a series of questions about patient-provider communication and information sharing. Furthermore, there is racial and ethnic inequity in patient experiences: Black and Hispanic women were among the least likely populations to report that their family planning provider was “excellent” on several measures, while White women rated their experiences with providers most highly.
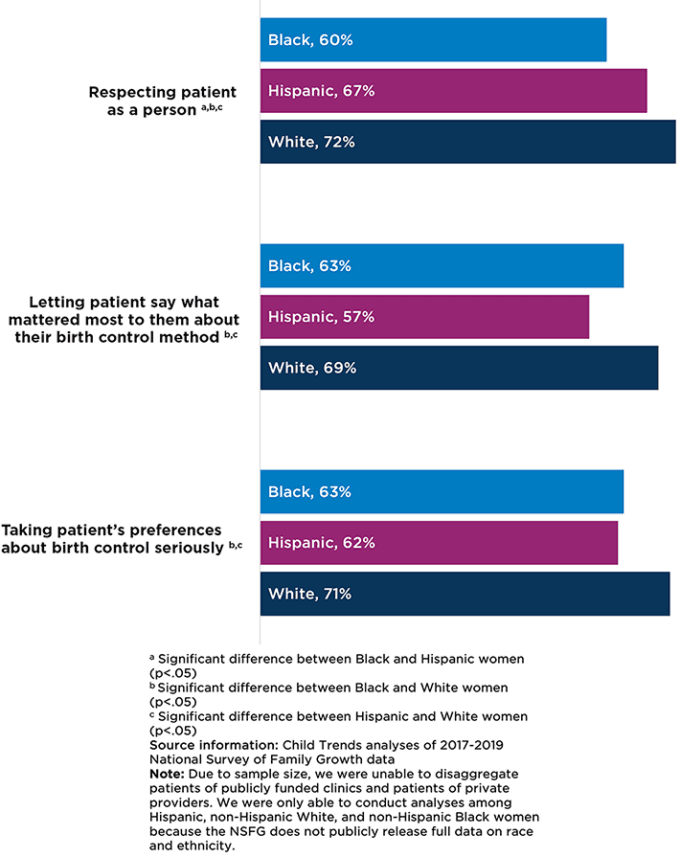
When asked to rate whether their provider respected them as a person, 60 percent of Black women, 67 percent of Hispanic women, and 72 percent of White women rated their provider as “excellent.” We also found that 63 percent of Black women, 57 percent of Hispanic women, and 69 percent of White women rated their provider as “excellent” in letting them say what mattered most about their birth control method. Finally, 63 percent of Black women, 62 percent of Hispanic women, and 71 percent of White women reported that their provider was “excellent” in taking their preferences about birth control seriously.
Percentage of family planning patients who rated their provider “excellent” on patient-provider communication measures, 2017-2019
White, Black, and Hispanic women were equally likely to rate their provider as “excellent” in giving them sufficient information about birth control. This suggests that the primary difference among women of different races and ethnicities was around the counseling and decision-making processes, rather than with the education that providers gave them about contraceptive methods.
Previous research suggests that racial and ethnic disparities in women’s experiences with family planning providers are due, in part, to providers’ racial biases: Primary care providers’ implicit racial biases can result in poor-quality patient-provider communication and lower patient ratings of interpersonal care, particularly for Black patients. In qualitative studies with family planning patients, Black and Latina women also report feeling implicit pressure from providers to use specific birth control methods and describe other negative experiences with contraceptive counseling, including impersonal counseling and poor communication. These negative encounters can have long-term reproductive health implications: A 2016 study found that women who reported lower interpersonal quality of care during a recent contraceptive counseling visit were less likely to still be using their selected method six months after their appointment. This is important because contraceptive discontinuation is linked to a greater risk of unintended pregnancy.
Providers can take proactive steps to reduce racial and ethnic disparities in patient experience and improve interpersonal communication and health outcomes for all women. The Reproductive Health National Training Center provides resources to help providers ensure that family planning care is voluntary, patient-centered, and noncoercive, including guidance on recognizing the history of coercive practices in contraceptive counseling and on guarding against coercion. Providers can improve patient experiences and improve reproductive health outcomes by using a patient-centered, shared decision-making approach to contraceptive counseling that focuses on listening to and addressing patients’ preferences rather than simply urging patients toward highly effective methods.
© Copyright 2025 ChildTrendsPrivacy Statement
Newsletter SignupLinkedInYouTubeBlueskyInstagram

