Early Evidence of Medicaid’s Important Role in School-based Health Services
In the midst of the COVID-19 pandemic, education and health officials need up-to-date information on the state policy landscape that affects billing for Medicaid services provided in schools. Moreover, it is crucial that these officials understand how policies may promote or impede health services provided in schools. To that end, Child Trends conducted a study to explore how shifting Medicaid policies have influenced access to school-based health services. This brief examines the following:
- Which states have policies that allow or restrict Medicaid billing for school-based services (Part 1)
- Whether differences in state policy influenced the availability of Medicaid dollars for school services (Part 2)
- State and local health and education officials’ early challenges and successes implementing new Medicaid policies (Part 3)
Download
Key findings
- As of Fall 2020, more than half of all states and the District of Columbia (26) had barriers inhibiting schools from utilizing Medicaid to support free school-based health services.
- From 2010 to 2018, state Medicaid expenditures on school-based health services increased, although we have yet to see the large changes we expected following CMS’ 2014 free-care rule change.
- States and districts were motivated to expand Medicaid-covered services given the potential to increase access to health care for students.
- State and district leaders see early investments in stakeholder engagement as helping them achieve a smoother implementation of new Medicaid policies.
- Local leaders often struggle with the logistics of implementing Medicaid-compliant billing systems and meeting licensure requirements for service providers.
Context
Too many children in the United States, including those enrolled in Medicaid, go without regular health screenings and preventative services. In 2018, only 56 percent of the 27 million children ages 3 to 18 who were eligible for Medicaid services received at least one initial or periodic physical, mental, developmental, dental, hearing, and/or vision screening. That same year, only half of adolescent Medicaid recipients received a comprehensive well-child visit. And although access to health care has become more equitable in recent years, gaps in care persist by race, ethnicity, and income. Nearly one in five Hispanic children have not had a well-child visit in the past year and nearly one in 10 have an unmet health need—higher percentages than for any other racial/ethnic group. In addition, children whose families live at less than 100 percent of the federal poverty level are six times more likely to have no usual source of care than children whose families live at more than 200 percent of the federal poverty level.
Schools are uniquely situated to address these challenges and to advance health and health equity, as they are critical partners in delivering screenings and preventative services for all children, including the nearly 36 million children insured through Medicaid (including the Children’s Health Insurance Program). School-based health services are especially important in the midst of the COVID-19 pandemic, when children and youth are reporting increased feelings of worry, depression, and disconnection.
However, not all schools have the capacity needed to provide these essential services. Currently, only about half of all schools have a full-time school nurse. Nurses are most common in schools serving affluent children and least common in schools in which 75 percent or more of children are approved for free or reduced-price lunch. Instead, for many schools, school-based health services and supports—including school nurses, psychological counseling services, audio and visual screenings, and school-based health centers—depend on funding provided by Medicaid. Medicaid is a joint federal-state program in which the federal government reimburses a state for a portion of its approved health expenditures (the average being 57%), so, Medicaid services require state investment.
While Medicaid provides key funding for health and preventative services, Medicaid policy may inhibit broader access to school-based health supports. Until recently, the so-called “free care” policy prevented schools from obtaining reimbursement for services provided to Medicaid-enrolled students that were available without charge to the beneficiary (including services that were available to the community at large). That changed in 2014 when the federal Centers for Medicare and Medicaid Services (CMS) released guidance—referred to as the free care reversal—clarifying that states may determine whether they allow schools to be reimbursed for services that would otherwise be available without charge. To take advantage of the federal changes, states could submit State Plan Amendments to change their State Medicaid Plans. Since the guidance’s release, nearly a dozen states have taken steps to expand Medicaid reimbursement for school-based health services. With states submitting and implementing amendments, a patchwork of state Medicaid policies has emerged to provide different coverage for different beneficiaries.
Part 1: Analysis of State Medicaid Policies
As of 2020, over half of all states have Medicaid policies that limit Medicaid billing for school-based health services.
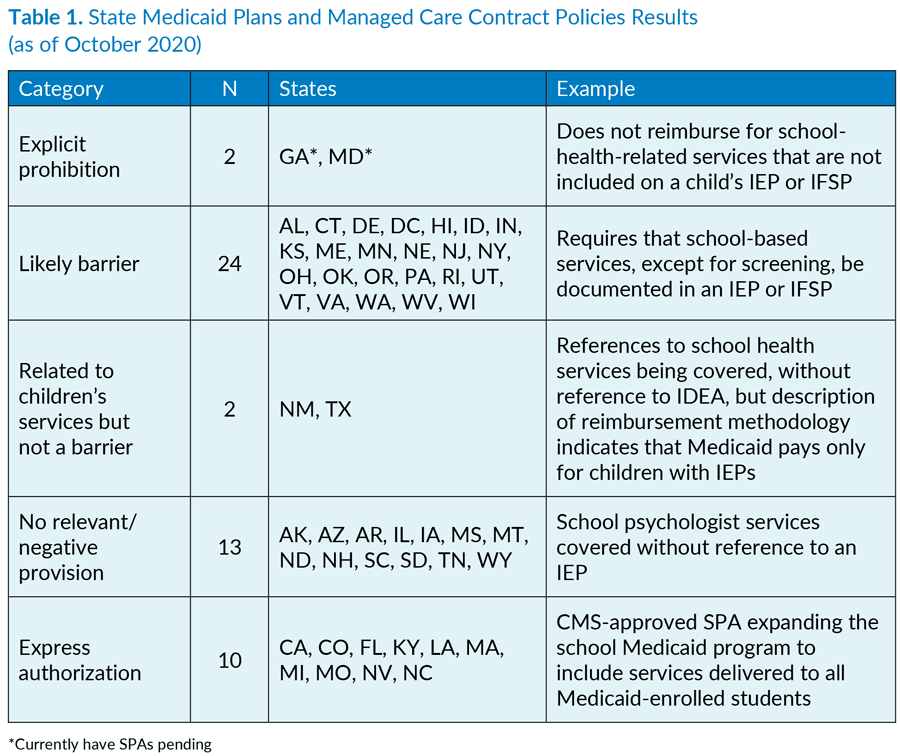
This policy analysis, which builds upon 2016 work from the National Health Law Program, examines State Medicaid Plans (SMPs), State Plan Amendments (SPAs), and Managed Care Contract Policies (MCCPs) in all 50 states and the District of Columbia (DC). Results indicate that, as of Fall 2020, more than half of all states and the District of Columbia (26) had barriers inhibiting schools from using Medicaid to support free school-based health services. These barriers generally limited Medicaid billing to health services specified in an Individualized Education Plan (IEP), or an Individualized Family Service Plan (IFSP), for youth served under the Individuals with Disabilities Education Act (IDEA). The remaining states (25) either expressly authorized the use of Medicaid for health services delivered to any Medicaid-enrolled student, or had provisions that seemed to allow for Medicaid billing without references to IEPs or IFSPs. When state plans or managed care contracts authorized school-based health centers to bill for services provided to Medicaid-enrolled students, states generally avoided the language “free care.” Instead, they referred to “school-based services,” “services provided in schools,” or services provided “in a school setting.”
State Medicaid Policy Documents
State Medicaid Plans (SMP): Comprehensive written state plans for Medicaid administration, approved by CMS, which serve as agreements for how states will run their Medicaid programs.
State Plan Amendments (SPA): Changes to existing State Medicaid Plans. States can update Medicaid plans by submitting a SPA to CMS for approval.
Managed Care Contract Policies (MCCPs): Contracts between a state agency and managed care entity, or requests for proposals for contracts, issued by state agencies, to managed care organizations for contracts to provide Medicaid services. These contracts and requests for proposals outline the various state requirements by which managed care organizations must abide.
In most cases, SMPs contained language about barriers or authorization regarding school-based health services. This language was less common in MCCPs; however, when it was present, the language resembled the restriction or authorization described in the SMP. Only Arizona’s and Tennessee’s MCCPs indicated a barrier to coverage of school-based services that was not already present in their SMPs. Nine states did not have managed care contract policies, while two did not have any managed care services for children. Hawaii’s MCCP was not included, as new contracts were awarded in January 2020 but subsequently postponed and rescinded by May 2020 due to the COVID-19 public health emergency. The results are summarized below in Table 1, following a brief explanation of how SMPs, SPAs, and MCCPs were coded. For specific state results, click here (PDF).
We coded SMPs, including SPAs, into one of five categories:
- Explicit prohibition: States that had specific barriers to covering Medicaid services provided free of charge, which include school-based services
- Likely barrier: States with provisions related to Medicaid services that could present a barrier to reimbursement for coverage
- Related to services for children: States with provisions related to Medicaid services that likely would not impede reimbursement for school-based services
- No reference: States with no provisions that would negatively affect coverage of Medicaid services provided in schools
- Express authorization: States providing express authorization for covering school-based services without limiting them to services included in an IEP or IFSP
Likewise, we coded MCCPs into one of four categories:
- Explicit prohibition: States that had specific barriers to using Medicaid for school-based services
- Likely barrier: States with provisions that could present a barrier to using Medicaid for school-based services
- No reference: States with no provisions that would negatively affect coverage of services
- Express authorization: States with express authorization for covering school-based services
Part 2: Analysis of State Medicaid Expenditures
Medicaid expenditures for school-based health services have steadily increased since 2010, but recent state policy shifts may need more time to exert an influence on Medicaid expenditures.
Medicaid expenditures for school-based health services have increased but we did not find a larger increase after 2014 or a larger increase for states that can receive reimbursement, relative to states that cannot. We analyzed Medicaid expenditures for shifts in billing for school-based health services from 2010 through 2018 (CMS’ rule change occurred in 2014). Our team also explored whether expenditures changed more significantly in states with policies allowing for reimbursement than in states with policies that do not allow for reimbursement. We hypothesized that more permissive Medicaid policies would generally lead to increases in expenditures on school-based health services.
This analysis used Medicaid financial and enrollment data to create a measure of a state’s expenditures for school-based health services per enrolled child for each year from 2010 to 2018. Data from 2019 through 2020 were not available for use in this analysis. This measure is commonly used to compare Medicaid expenditures between states, which have large variation in the size of their enrolled populations. In 2018, the number of children enrolled in Medicaid averaged roughly 700,000, ranging from 40,000 in Wyoming to over 4.5 million in California. Expenditures on school-based health services averaged $114 million and ranged from $450,000 in Oklahoma to $1.3 billion in Texas. The ratio of expenditures on school-based health services per enrolled child makes for more manageable numbers: Expenditures per enrolled child averaged $162 in 2018 and ranged from $87 in Oklahoma to $650 in DC.
Expenditures for school-based health services per enrolled child are available below, for all states and Washington, DC from 2010 to 2018.
State Medicaid Expenditures on School-based Health Services per Enrolled Child, by Potential Policy Barriers
This analysis has important limitations that may have affected our ability to detect our hypothesized relationship. First, our analysis only captured four years of data since the release of the free care reversal guidance; additional years of data may be necessary to detect the guidance’s effects. Some of the first states to take advantage of CMS’ rule change in 2014 were still training their staff and preparing for implementation at the district and school levels in 2020. If we were to repeat this analysis in two to three years, we would perhaps detect a change. Second, our data did not permit us to distinguish between expenditures for free care and other school-based health services. This means that increases in services for children with disabilities served under IDEA could increase expenditures on school-based health services, as could increases in free care. Finally, states only began to report expenditures specifically for school-based health services during our study period, and generally varied in how quickly they began to report these expenditures separately. This added further variability to data that already greatly fluctuate from year to year.
Part 3: Views of Education and Health Officials, State and Local
Education and health leaders in the early stages of expanding school-based Medicaid programs report signs of increased access to health services, but note ongoing challenges with navigating Medicaid paperwork burdens and supporting providers.
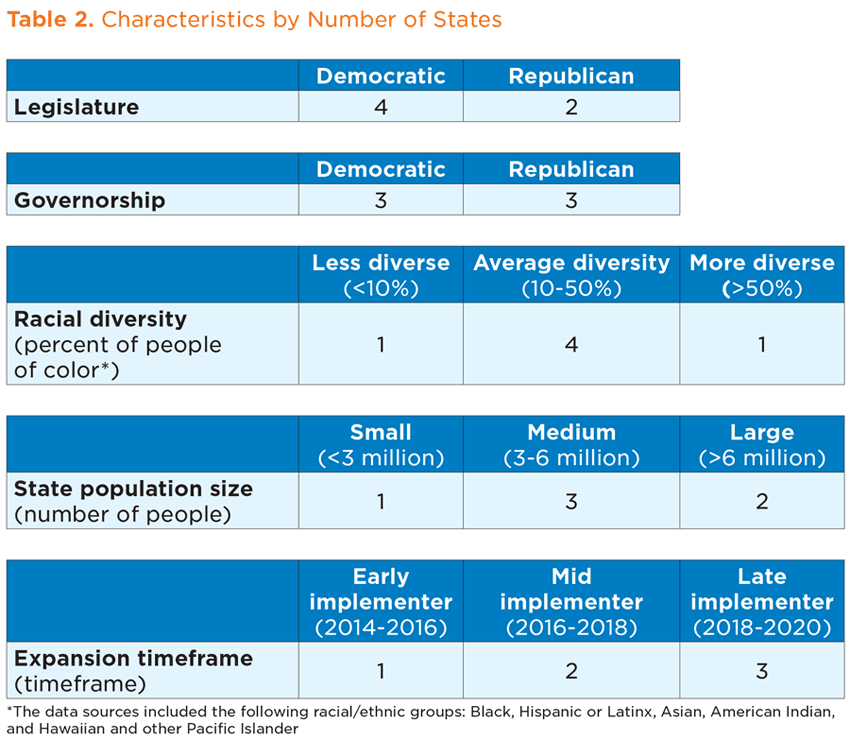
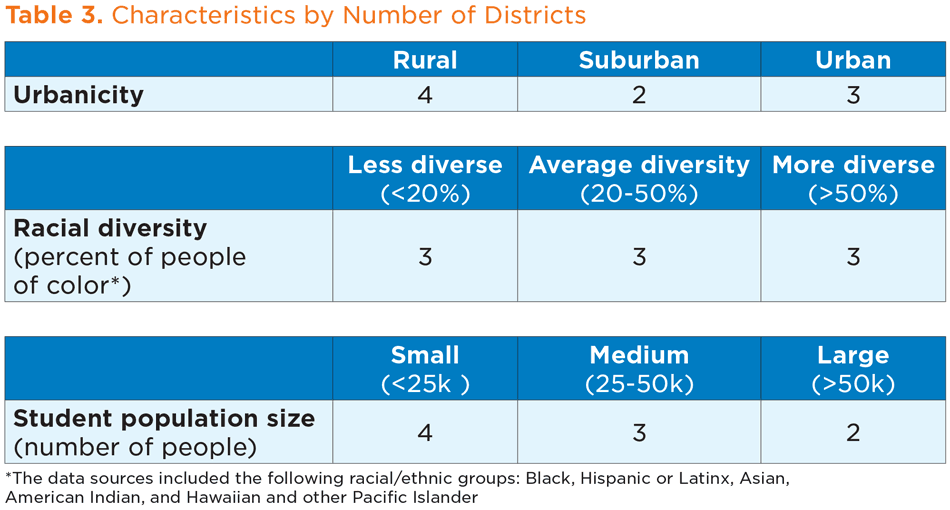
From Fall 2019 to Summer 2020, Child Trends spoke with representatives of state health and education agencies in six states, as well as individuals responsible for managing Medicaid reimbursement in nine districts from within three of these states. Tables 2 and 3 outline the characteristics of the states and districts, respectively, that participated in our study.
We began the study focused on free care—reimbursements for eligible services that might be available at scale and free of charge in the community, such as health screenings. However, state leaders described the federal reversal in free care policy as the catalyst for a shift toward expanding eligible school-based services beyond those provided under IDEA. Consequently, we expanded our framing of recent state policy shifts to align with what we were hearing from state leaders.
Because Medicaid is a partnership between states and the federal government, each state’s experiences are different. Similarly, experiences can vary dramatically across communities within the same state. This summary focuses on themes that emerged in multiple of our 19 interviews, suggesting that these themes might be relevant for other states considering changes to Medicaid reimbursement for school-based health services.
States and districts were motivated by the potential to increase access to health care and realize early signs of progress
“If I have an affluent school district that can pay their social worker 30% more than what an economically disadvantaged school district, where does that social worker go? They go to the more affluent school district. […] That’s something that we’re trying to address by authorizing more providers to perform these services thinking out of the box a little bit.” – State Leader, State Department of Health and Human Services
The primary motivator for states and districts pursuing an expansion of Medicaid support for school-based health services was to improve access to services—particularly behavioral and mental health services—for students. Some states and districts also mentioned their hope that expanding services would reduce health disparities, although only one district described health equity as an explicit motivating factor. Most local leaders stated that their initial goals were to obtain reimbursement for health services that they were already providing to general education students enrolled in Medicaid—especially behavioral health.
While several jurisdictions were still early in their expansion process, state and local representatives reported progress on these initial milestones. While recognizing that children’s needs—especially behavioral health needs—continue to outweigh the availability of providers in their communities, nearly all local leaders noted that students had already received additional services. Both state and local representatives were also hopeful for increased funding, but most emphasized that it was too early to know how much funding they would receive in a full fiscal year, or whether funding would be adequate to pay new salaries. For information on how states are leveraging telehealth to better provide behavioral health services amid the pandemic, see this blog post.
State leaders see early investments in stakeholder engagement paying off, while local leaders continue to address concerns from clinical and administrative staff.
“We had workgroups going that actually include most of our experienced school districts to get their input because I firmly believe that if you write a policy in a vacuum, you get bad policy. So we had schools go on every step of the way. We had some of the people that were closely connected to the legislature.” – State leader, State Department of Health and Human Services
State and local leaders reported different experiences engaging stakeholders and establishing buy-in. Among state leaders, stakeholder engagement generally involved engaging diverse coalitions of stakeholders who, for their own unique reasons, encouraged and supported the expansion. States whose legislatures were involved in the process emphasized the value of having an array of supporters when facing political obstacles and pushback. State leaders also described efforts to secure buy-in from district-level implementors and providing school administrators with direction.
While local leaders described establishing buy-in from clinical and administrative staff, many local representatives reported challenges with maintaining buy-in as staff became frustrated with the increase in time dedicated to billing documentation. This has been especially true among clinical staff who prefer to prioritize their time delivering services. Local leaders also explained that some clinical staff feel that their new responsibilities related to medical billing and diagnosis feel better suited to the medical field—and that these responsibilities were a poor fit for their expectations in school-based health.
Investments in clear guidance and ongoing communication can be challenging but can result in better collaboration and smoother implementation.
“We’ve made a very concerted effort to reach out to the school districts … to allow them the opportunity to have a voice in development of new administrative rules, to provide education to them around what it means to be a qualified Medicaid provider, and all the implications that go along with that. We made a commitment to the stakeholders that we would hold regular sessions for them.” – State leader, State Department of Health and Human Services
To facilitate the expansion, state health or Medicaid agencies provided trainings and guidance documents for education personnel, including implementation guides and documentation templates. Many state leaders described efforts to share guidance with local leaders well in advance of implementation. Some state and local leaders mentioned holding regular workgroups, meetings, and conferences to support the learning process. In addition to raising awareness about the expansion, these meetings had very tangible benefits. For example, some local leaders described sharing or receiving templates for required documentation, including plans of care, which helped streamline their implementation planning.
State and district leaders discussed the benefits of investing in communication to improve relationships between state and local agencies, and of greater collaboration across health and education sectors. For example, we heard about requests for technical assistance made by local leaders to state agencies resulting in improved collaboration and relationships with the health or Medicaid agency.
Local leaders often struggle with the logistics of implementing Medicaid-compliant billing systems and meeting licensure requirements for service providers.
“But that’s been some of the challenge is that the systems that support billing weren’t really ever set up for [general education] students. So that has required some retooling or expansion of programs to be able to do that.” – District leader
As noted earlier, nearly all local leaders shared examples of challenges with shifting to Medicaid-compliant billing systems. Most local leaders described delays in setting up new billing systems, which meant that providers were not able to log in their services right away. Many local leaders talked about additional delays in obtaining parental consent forms to comply with the Family Educational Rights Privacy Act (FERPA). Several also noted that they had not anticipated the amount of time that would be needed to create medical record documentation that aligns with their state’s Medicaid plan for services that were not previously reimbursable. In some cases, local leaders noted that state agencies had provided them with templates; others described adapting or adopting forms used by other districts, while still others explained that they simply had to develop their own forms. Most leaders agreed that creating forms is time-consuming and can be challenging without clear guidance on whether the forms are Medicaid-compliant.
Some local leaders noted that providers already have significant responsibilities, and that the additional work of billing for services has resulted in some pushback against the expansion. Further confusion around the requirements for documentation to bill—as a result of conflicting information from state education and health agencies, according to local leaders—has made it difficult to gain buy-in from some providers who feel they are losing time that would be better spent seeing students.
Local leaders reported another significant barrier: identifying practitioners who meet licensure requirements to bill for Medicaid—particularly for behavioral health. This challenge was particularly difficult for rural districts, many of which were already dealing with staffing shortages. Moreover, local leaders explained that, even when a qualified practitioner is identified or hired, the process to add them to the staff pool list can be time-consuming. For more information on how states are navigating these licensure barriers, see this blog post.
Establishing efficient and compliant processes and systems can lead to early successes.
Some local leaders described an unexpected benefit to the increased attention to medical billing: greater knowledge of and confidence about their billing processes. For example, some reported identifying billing procedures that were either being done incorrectly or that could be done more efficiently. We also heard that feedback from local education leaders sometimes pushed state agencies to update their policy manuals to better meet the needs of individuals implementing the changes in local communities.
Conclusion and Recommendations
CMS’ free care reversal in 2014 lifted restrictions on billing Medicaid for services provided in school settings. Many states have exercised their new flexibility to expand Medicaid reimbursement, leading to a patchwork of Medicaid policies providing different degrees of support for school-based health services: Just under half of all states now have SMPs that allow reimbursement for eligible services, for eligible students, without restrictions. We sought to study these changes in state plans and their implications for school health capacity and health equity. At the outset of our work, we assumed that health equity would be a driving motivator for states to pursue an expansion of health services in schools; as a result, we asked about this factor in all interviews. Surprisingly, health equity was largely absent as a motivator for states, but with a collective and newly heightened awareness of systemic inequity, it may emerge as a motivator for other states considering this change.
While our study did not find that more lenient state policy provisions were linked to increases in Medicaid expenditures, it is possible that states are too early in their implementation of new policies. For now, interviews with state and district personnel provide an early glimpse of the opportunities and challenges of expanding Medicaid reimbursement. The following five recommendations emerged across our analyses and interviews:
Engage leaders from state health and education agencies early in the process.
During planning for expansion, include leadership at both the state Medicaid and education agencies, as well as the relevant legal department; the latter can ensure adherence to federal regulations, as other agencies may be unaware of federal regulations such as IDEA guidelines. Also include staff from health and education departments, whose recommendations should inform decisions on the expansion roll-out.
“…we would rather get that stakeholder input and that collaborative approach from the beginning than try to play catch up on the back side. And so I think that what that does, also, is that it sets you up so that you can move forward on that and the policy changes, you’re not also simultaneously fighting those political battles that are bound to come, right?” – State leader, State Department of Education
Build relationships with community and advocacy organizations.
Gather consensus and input on expansion efforts from inception. In situations involving pushback, use data to communicate the need for expansion.
“So being able to say, ‘Look, our kids are hurting’, and using data from the YRBS, using data from the suicide attempts and completions and those kinds of things. So using the data to structure your message and not giving up despite the roadblocks that you’ll face because it’s important work.” – State leader, State Department of Health and Human Services
Reach out to CMS for guidance.
CMS can provide guidance on redirecting state efforts toward success, especially when drafting and approving the state plan amendment.
“Yeah. Used to be, ‘Oh no, this doesn’t work.’ Now they’re saying, ‘Well, this doesn’t work, but if you do this, it will.’ That’s helpful. I mean, huge. So I would say the big thing is to– that I’d like other states to know is that when you turn in a state plan right now, CMS seems to be trying to help you make it work so that it’s approved.” – State leader, State Department of Health and Human Services
Don’t rush; consider implementation approaches that allow for adequate planning and buy-in.
Design an extended planning process to assist LEAs in preparing for the expansion. This process could include creating a common language between the health and education spaces, engaging district business managers and superintendents to discuss the potential benefits of expansion, informing and educating parents about the expansion, and creating documentation and forms that serve the purposes of both Medicaid and school districts.
“I would consider giv[ing] yourself at least a year. Bring in your stakeholders and that would include your school district staff, and anyone else in your community that it will ripple-effect and touch, and sit down and figure out the game plan. […] Maybe start with a pilot program.” – State leader, State Department of Education
Proactively address potential stumbling blocks for local communities.
Increased funding may be insufficient to improve student access to care if there is a gap in available licensed health professionals. Strategies to address these gaps may include providing support for currently employed staff to obtain required credentials or working with graduate schools to create a workforce pipeline. Medical documentation requirements can also be challenging for district implementers. To mitigate this, states can provide templates to districts or encourage them to disseminate working templates to other districts. Health agency personnel can also review district forms and templates for compliance.
“…we tend to all help each other out rather than “Let’s have 56 different plans of care.” We don’t work that way. There are a couple of key people [who would say] “Look, I’ve got a plan of care, let’s put a template out on our Medicaid Dropbox. And so we can all work off from it. Let’s all review it and add or delete what we need or don’t need.” So we try to kind of work harder– or smarter not harder in that way.” – District leader
The states that have made changes to Medicaid reimbursement for school-based health services have only recently begun to implement those changes, meaning that it is likely too early to accurately quantify increases in funding or improvements in student health related to those efforts. However, despite the logistical challenges in rolling out policy changes to expand Medicaid reimbursement, state and district leaders interviewed for this study emphasized the promise of such efforts for increasing access to critical health services for children and youth. Given the outsized role of Medicaid as the largest child health insurance provider in the country, we encourage state and district leaders across the education, health, and social service sectors to consider the potential benefits of expanding Medicaid reimbursement for school-based services. Below are links to additional resources to provide further information.
- Healthy Students Promising Futures https://healthystudentspromisingfutures.org/topics/free-care-policy/
- National Association of Medicaid in Education https://www.medicaidforeducation.org/
- AASA: https://www.aasa.org/medicaid/
The project team would like to acknowledge that this work is supported by a grant from the Robert Wood Johnson Foundation [grant ID 76094]. We would also like to thank both our partner (the National Health Law Program) and Judi Wallace of Fairbanks, LLC for their contributions to this work.
Download
Authors
© Copyright 2025 ChildTrendsPrivacy Statement
Newsletter SignupLinkedInYouTube





