This brief highlights the current health care needs, access to health care, and health care experiences of Black families with children living in the South Ward, a predominantly Black community in Newark, NJ (see the text box “Defining Black,” adapted from a previous Child Trends brief). It also provides lessons learned and recommendations for policymakers, health care providers and practitioners, and other organizations and stakeholders interested in addressing the health care needs of Black families in the South Ward or other areas with similar characteristics.
The brief begins with an overview of the South Ward Promise Neighborhood (SWPN) initiative, including its goals and priorities. This section also describes the South Ward community, including an overview of residents’ health care needs. Following the community and resident summary, we explain our methods; then, we discuss findings from two data collection efforts that informed our understanding of the heath care needs of South Ward residents. We conclude the brief with early lessons learned to strengthen health care access and quality for Black families living in the South Ward.
Our key findings indicate that a number of South Ward families experience limited access and barriers to receiving health care; encounter racist, discriminatory, and unfair practices within health care systems and by medical providers, resulting in dissatisfaction with the quality of care they receive; and look forward to full implementation of the SWPN’s new community health center. We recommend that policymakers, practitioners, and other SWPN health stakeholders use the Promise Neighborhood’s community infrastructure to facilitate residents’ access to health care; seek out and use community input to inform respectful, culturally responsive care for residents; and engage in professional development and continuous learning.
Download
Defining Black
When referencing Black people throughout this issue brief, we are referring to individuals who may identify as African American—those who were primarily born in America and are descended from enslaved Africans who survived the trans-Atlantic slave trade—as well as the smaller populations of people living in America who may identify as Black African or Afro-Caribbean.
Black also includes individuals who reported being Black alone, or in combination with, one or more races or ethnicities in their responses to the U.S. Census Bureau American Community Survey, as well as in surveys conducted for this brief. For instance, this could be an individual who identifies as Black only, as well as someone who identifies as Black and White, combined, or Afro-Latino.
For simplicity, we report an individual or groups of people as Black if the data source category drawn on was labeled “Black or African American.”
Overview of the South Ward Promise Neighborhood and South Ward Residents
The South Ward Promise Neighborhood Initiative aims to provide high-quality schools and supports to residents of Newark’s South Ward.
The SWPN is part of a national Promise Neighborhoods (PN) initiative funded by the U.S. Department of Education. This five-year initiative was conceptualized to provide access to high-quality schools and coordinated systems of support for families living in communities that have been historically under-resourced in the United States. The PN initiative’s overarching goal, as described by the Department of Education, is to “significantly improve the educational and developmental outcomes of children and youth” in PN communities by preparing them to “attain an excellent education and successfully transition to college and a career.”
In 2017, the Building Resilient Intelligent Creative Kids (BRICK) Education Network (BEN) was awarded a $30 million Promise Neighborhood Grant.[1] As part of the application process, New York University conducted a neighborhood assessment to understand the strengths, needs, and resources available in the South Ward’s potential PN community. In addition to informing the PN grant application, neighborhood assessment data were also used to guide the development of PN goals and to inform the SWPN’s benchmarks of success. Since its inception in 2017, the SWPN’s priorities have included a focus on early care and education (ECE), college and career readiness, and housing. As the PN work has unfolded in the South Ward, health has also become an area of focus.
The Child Trends/BRICK Education Network Partnership
Child Trends is the external evaluator for Phase 1 (2017–2022) of the SWPN. This issue brief is borne out of the collaboration between Child Trends and BEN, a community-based organization that leads the SWPN. In addition to the Child Trends/BEN partnership, agencies working under the SWPN umbrella (i.e., partner agencies) helped recruit participants for this evaluation effort. Currently, there are more than 25 partner agencies, including those with a focus on early care and education, housing, and physical and mental health connected to the SWPN initiative.
Key features of the SWPN initiative and evaluation are its focus on implementation science and commitment to centering racial equity. This focus is made up of programming and evaluation strategies that include, but are not limited to, attention to the South Ward community history and context; inclusion of community engagement, voice, and strengths; and capacity building. From the outset, Child Trends and the SWPN mutually agreed that utilization of implementation science and racial equity frameworks—and a focus on the ways in which systematic racism has affected and continues to affect the South Ward community—would need to be front and center in designing the PN initiative, as well as the evaluation. Child Trends and the SWPN also understood that implementation of the SWPN’s services would need to be iterative and include opportunities to pilot, test, and solicit feedback on strategies to get them right. These tenets evolved from the longstanding core values of each individual organization and informed initial and ongoing meetings about project planning. Throughout project planning, the organizations ensured that attention was given to systems, institutions, and policies, and to the ways in which these factors and implementation processes could facilitate or hinder the advancement of Black families. In short, the team believed it was critically important that the South Ward community residents—who are majority Black and whose city has a history of social and health services disinvestment—were not marginalized in PN implementation or evaluation processes.
The SWPN Initiative Centered Implementation Science and Racial Equity Frameworks
Centering implementation science and racial equity in programming and evaluation is not a “one size fits all” proposition. In the SWPN initative, this occurred in a number of ways. For instance, we solicited and incorporated diverse community voices into the SWPN’s processes and services (i.e., creating and regularly engaging with community members and the SWPN advisory board) and used the feedback gathered to inform the program and evaluation. We supported the building of community capacity (e.g., training of the SWPN staff and residents in community surveying and data collection techniques); used rapid cycle evaluation and dissemination strategies to ensure ongoing feedback to SWPN agencies, programs, and the community (e.g., creating slide decks for community schools and fact sheets on community survey findings); and kept history, context, race, equity, and systems issues at the forefront of the project (e.g., regularly reflecting on research questions and data collection efforts to assess issues such as whether research questions accounted for the community’s historical, racial, and cultural context; considering who should be involved in data collection processes; and grappling with how much weight to give to specific data, etc.).
South Ward neighborhoods face challenges around health care access.
The South Ward is situated in the southwest corner of Newark, a city within Essex County, New Jersey. This small community consists of four neighborhoods: Upper Clinton Hill and Lower Clinton Hill in the north, Weequahic in the middle, and Dayton in the south. For our evaluation analyses, we used seven census tracts in the Upper Clinton Hill and Dayton communities as a proxy for the entire South Ward neighborhood (Figures 1 and 2).[2] This area is divided into two by a highway and, according to U.S. Census and American Community Survey (ACS) data, was home to 20,402 people from 2016 to 2020. During the same time period, 88 percent of the individuals living in the area were Black (regardless of ethnicity, including those who identified with multiple races) and 18 percent were foreign-born. Across the entire city of Newark, 24 percent were children under age 18.
On average, almost one third of families in the South Ward experienced poverty from 2016 to 2020 (Table 1). During the same time, in Newark, 23 percent of adults and 9 percent of children did not have health insurance (Table 1). Despite being a relatively small community with a large hospital (i.e., Newark Beth Israel Medical Center [NBIMC], with 667 beds) and three Federally Qualified Health Centers (FQHCs)[3] (Newark Community Health Center, George Washington Carver School, and Shabazz High School) nearby (see Figure 2), research conducted in Newark and with South Ward residents[i] indicated the need for more health care providers (e.g., primary physicians, dentists, mental health professionals, etc.) in the neighborhood. In fact, the Dayton neighborhood, located in the southern part of the South Ward, was recently designated by the federal Health Resources and Services Administration (HRSA) as a Medically Underserved Area (MUA).[4] Additionally, as of 2017, the South Ward did not have any retail-based health care options,[5] a service with the potential to fill voids in health care access, especially for individuals without insurance.
U.S. Census Bureau American Community Survey (ACS) data
Most ACS data for the South Ward tract presented in this brief are unreliable due to small sample sizes. However, this is the best publicly available source of information to understand the hyper-local context of the South Ward. Data should be interpreted with extreme caution. We also present each data point at the Newark level (Table 1), as data at the city level are more reliable.
Table 1. Demographic and health data of South Ward and Newark residents, by percentage
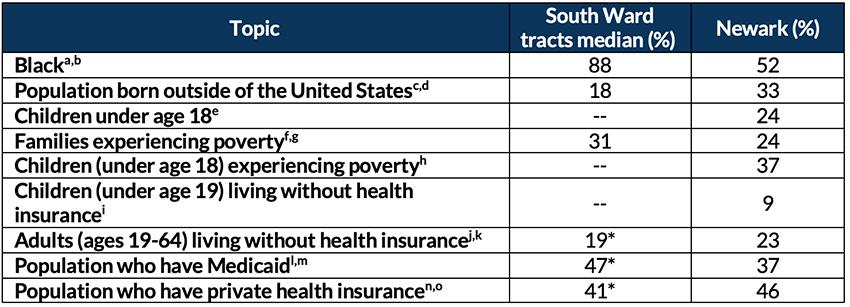
Note and Sources
Figure 1. Locations of health facilities in Newark and South Ward
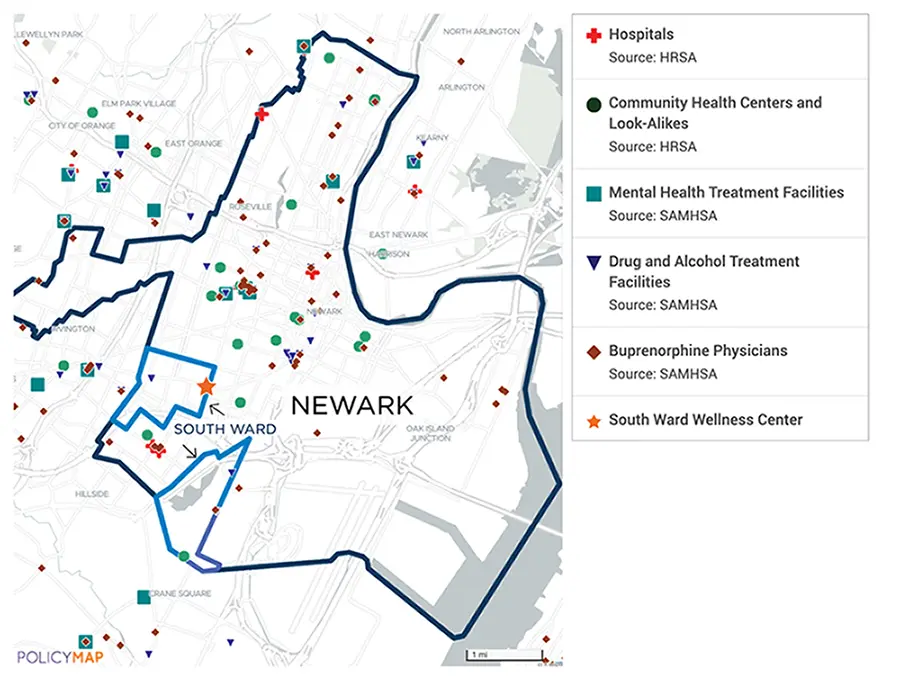
Note 1: The blue boundary represents the South Ward and the navy boundary represents the City of Newark.
Note 2: The two hospitals (red crosses) between South Ward neighborhoods both represent NBIMC (one hospital).
Note 3: Community Health Centers are equivalent to FQHCs. “Look-alikes” operate similarly to FQHCs, as well, and can apply to receive benefits such as enhanced Medicare and Medicaid reimbursement.
Source: HRSA and Substance Abuse and Mental Health Services Administration (SAMHSA) data from PolicyMap
In response to the need for more hyper-local health care options, and to better understand how South Ward infants and young children are faring before they enter primary school, the SWPN initiative partnered with St. James Health, a community-based health care services organization, to launch the South Ward Wellness Center (the Center). The Center opened its doors in 2022 and has an FQHC designation. The Center is currently in the early stages of development and has been conceptualized as a one-stop shop for preventative health care services for adults and children living in the South Ward, although it will prioritize birthing people and children for services. In alignment with the SWPN’s goals, the Center will provide access and referrals to a wide variety of social supports, including assistance with enrolling in Medicaid.
Figure 2. Locations of South Ward neighborhood health facilities (zoomed in)
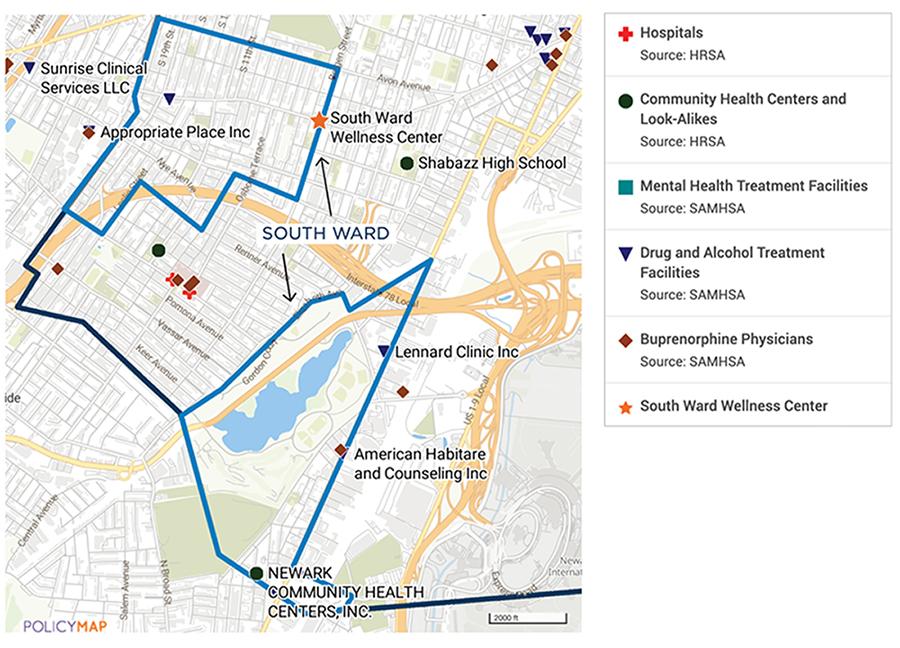
Source: HRSA and SAMHSA data from PolicyMap
Methodology
In this section, we describe the two data collection efforts that informed this brief. The first, a community survey, was designed to facilitate understanding of South Ward families’ demographics; overall well-being; and their access to, use of, and opinions about technology, education, child care, employment, housing and health services, supports, and resources. We also asked family respondents about how the COVID-19 pandemic had impacted their lives, and about their experiences with racism and discrimination in the South Ward.
The second data collection effort involved recruiting a small number of South Ward families and stakeholders working in health-related fields and asking them open-ended questions to better understand processes related to families’ specific health care experiences in the South Ward. Through the interview questions, we explored topic areas such as the interviewees’ backgrounds; their access to primary, specialty, and other health care services; their barriers to receiving health care services; how factors such as race, gender, geography, and class affected their experiences of receiving health care services; their processes for making decisions about using health care providers; the perceptions of the availability of children’s mental health services; and their perceptions about the Center.
The community survey
The community survey for the SWPN initiative was conducted from Winter 2020 through Spring 2021, which coincided with the middle of the COVID-19 pandemic. In November 2020, we sent postcards to South Ward addresses (N = 23,230) using the U.S. Postal Service’s Every Door Direct Mail program.[6] In March 2021, we conducted additional targeted outreach, in collaboration with the SWPN’s partner agencies, to increase the number of Black South Ward residents responding to the survey. Participants responded to the survey online or by phone.
The survey generated a total of 338 eligible responses from residents who lived in the zip codes of interest in and around the South Ward catchment area.[7] For this brief, we have limited reporting to the 165 residents who identified as Black. Table 2 provides a summary of the demographic characteristics of the 165 respondents.
Presenting the Data
When describing the survey data in this brief, we indicate the response size in parentheses. For example, when we say, “Seventy-three percent (N = 115) of parents or caregivers in the South Ward reported having a usual source of care for their children,” we mean the following: Of all people who responded to this survey question, excluding those who skipped the question or responded “Do not know” or “Do not wish to answer,” 73 percent, or 115 people, noted that they have a place they usually go when their children are sick or when they need advice about their health. Notably, the denominator does not always equal the full sample of 190.
When the findings are presented as charts, we note the full sample size (total number of people who responded to the question) after the title.
Finally, to maintain the anonymity of the respondents, we excluded survey findings when the number of responses was less than 10. We also removed revealing information from the interview quotes to protect interviewees’ identities.
Table 2. South Ward community survey demographics (N = 165)

Note: We suppressed the numbers with less than 10 respondents for privacy concerns. They are noted as “- -“.
Resident and stakeholder interviews
To better understand the South Ward context, we held in-depth interviews with three caregivers of children under age 18 who identified as Black, and with three stakeholders who work on health-related issues in the South Ward. Participants were recruited for interviews with the help of SWPN staff. We conducted all interviews by phone from December 2021 to February 2022 (a timeframe concurrent with the COVID-19 pandemic’s Omicron wave) and had a lead interviewer and notetaker on each call. We also recorded each interview so the research team could reference the recording if we needed additional clarity about the interview content. Interview notes were thematically analyzed using Microsoft Excel, and select members of the research team triangulated the interview content and themes.
Findings
In this section, we present findings from four key areas of the South Ward community survey and in-depth interviews:
- Families’ lack of access to primary care
- Families’ barriers to accessing health care
- Caregivers’ dissatisfaction with the quality of health care they received, citing racism, discrimination, and unfair practices as contributing factors
- Anticipation that the South Ward Wellness Center will fill a health care void
For each finding area, we share select research studies that provide relevant context for the findings. We then highlight survey data and, when applicable, interview data to further illuminate the theme.
A sizable number of South Ward families lack access to primary care.
An adult having a usual source of health care—a medical professional or health facility they can go to when they are sick or need medical advice—is a characteristic associated with them receiving critical preventive services, such as breast cancer screenings, and with their perceptions of higher quality of care. For children, having family-centered, coordinated, and ongoing health care has been shown to improve health care utilization, support more positive health outcomes, strengthen the quality of care for children, and reduce financial burden for families.
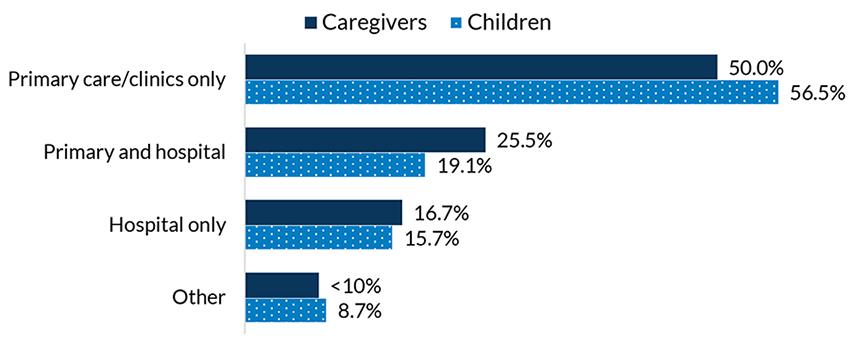
Seventy-three percent (N = 115) of parents or caregivers in the South Ward reported having a usual source of care for their children, and 65 percent (N = 102) reported having access to a usual source of care for themselves. Among respondents who reported having a usual source of care for their children, 83 percent (N = 95) reported using primary care or clinics for their children, and 82 percent (N = 84) reported using primary care or clinics for themselves. These facilities include doctors’ offices, clinics or health centers, school health providers, and urgent care facilities or retail-based health clinics.[8]
Almost one in six, or 16 percent (N = 18), of caretakers with a usual source of care for their children reported only using the hospital (emergency room or outpatient department) for their child’s health care needs, and 17 percent (N = 17) utilized only the hospital for themselves (see Figure 3). Moreover, 27 percent (N = 42) of caretakers reported that their children did not have a usual source of care at all and 35 percent (N = 54) reported the same for themselves. It is also likely that these caregivers and children without a usual source of care rely on hospitals as their main source of care, a finding that is consistent with research that suggests not having a usual source of care leads to higher emergency room utilization. For Newark residents in particular, using the emergency department as a primary source of care was noted as common in a previous study, in part because of the lack of primary care physicians in the region.
Figure 3. Places children and caregivers go for health care, among those who have a usual source of care (N = 102 for caregivers, N = 115 for children)
A portion of South Ward families experience barriers to accessing health care.
As indicated in Table 1, about 31 percent of families in the South Ward—and just under 37 percent of children under age 18 in Newark—were experiencing poverty from 2016 to 2020. Through the South Ward community survey, we found that 24 percent of respondents (N = 38) were unemployed at the time of the survey (late 2020 to early 2021) and 66 percent of respondents (N = 104) had experienced a loss of employment income since the start of the COVID-19 pandemic. Research shows that unemployment is associated with poor health outcomes. There also appears to be a link between health insurance and employment, whereby having affordable health insurance and health care may increase employment, but being employed does not always lead to having affordable health insurance. This issue is especially salient for people who work for low wages.
Whether related to socioeconomic or employment status, a lack of income is an important Social Determinant of Health (SDoH)[9] that can influence factors such as where and how one lives; one’s diet, nutrition, physical activity, psychological functioning, and other health-relevant factors, such as exposure to environmental pollutants; whether one can access transportation to get to a job; one’s school, child care, or health care facilities; and one’s ability to pay for health services. In fact, a Health Care Debt Survey conducted by the Kaiser Family Foundation in Spring 2022 found that over half (60%) of Black adults reported difficulty affording their health care costs. In the South Ward, 25 percent of community survey respondents (N = 38) reported missing a medical appointment for their children in the past year, with 55 percent (N = 21) citing financial reasons as the cause. Other reasons for missed appointments included a lack of health insurance (45%, N = 17), fear of COVID-19 exposure (34%, N = 13), and a lack of transportation (<25%, N < 10) (see Figure 4).
For caregivers themselves, 34 percent (N = 54) reported having missed a medical appointment in the past year. Of those, 44 percent (N = 24) noted financial issues as their reason, followed by a fear of COVID-19 exposure (35%, N = 19), lack of health insurance (30%, N = 16), lack of child care (28%, N = 15), and lack of transportation (19%, N = 10) (see Figure 4).
Figure 4. Reasons medical appointments were missed, for caregivers and children (N = 54 for caregivers, N = 38 for children)
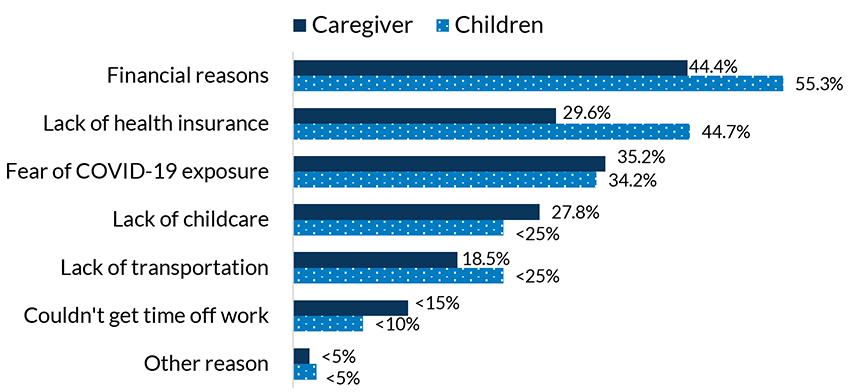
Note: Percentages add up to over 100 percent because respondents were able to select multiple options.
Nearly all interviewees cited the dearth of medical providers as a challenge in the South Ward. The shortage resulted in a lack of available appointments, providers not accepting new patients, and people having to wait long periods of time to be seen by medical providers.[10] Interview participants also reported that appointments often had to be scheduled far in advance, which posed challenges if unanticipated health care issues arose such as the need for sick visits, a likely occurrence given the ongoing presence of the COVID-19 pandemic. Caregivers also noted that medical provider shortages were exacerbated by the COVID-19 pandemic, which has made it especially difficult to keep up with their child(ren)’s medical appointments. Fear of contracting COVID-19 while visiting providers (a finding also noted in the community survey) and crowded waiting rooms without adequate space for social distancing were also deterrents to accessing health care. One caregiver shared:
“I will say that they’re definitely overbooked, because if you walked into one of those offices, and I’ve been there during COVID, it was as if it was pre-COVID. Not that people weren’t wearing masks, but the seats weren’t placed apart.”
Interviewees also noted concerns about a lack of specialty care providers in the South Ward. One resident noted:
“In terms of health services, there are not a lot of eye doctors and dentists near me. That would be helpful. Currently, my dentist is in [nearby town] that is where I take my kids. In general, it would be helpful to have more specialty doctors near me.”
In addition to the lack of providers to address physical health concerns, respondents cited the absence of mental health resources, particularly for children, as an ongoing challenge in the South Ward. One stakeholder shared:
“There isn’t really a place that addresses [the] mental health needs of children in the South Ward. I usually have to connect them to our counselor or licensed clinical social worker who then talks to the mom … and then has to get permission to talk to the 17-year-old …There was one in downtown, but you have to have insurance. You know, you have to fill out this huge application. You have to wait to be accepted. There may be a waiting list …”
Immigration status and language were also cited as challenges to health care access. For Black African immigrants, being undocumented was a risk for lacking access to health insurance. In addition, two stakeholders noted immigrant patients’ difficulties finding providers who spoke their same language, and one person reported witnessing discriminatory treatment of people at health care facilities who did not speak English. Given the fact that about one fifth of South Ward residents were born outside of the United States (see Table 1), this issue is one that warrants attention.[11]
Some caregivers were dissatisfied with the quality of health care they received, citing racism, discrimination, and unfair practices as contributing factors.
Racism is a considerable factor in determining how health care is delivered and accessed in the United States. This includes centuries of egregious and unfathomable behaviors such as medical experimentation and infringements on Black people’s bodily autonomy, as well as violations of their informed consent.[ii] Racism can also result in interpersonal discrimination that affects how Black people access and experience health care. A 2017 literature review examining associations between racism and health care use concluded that experiencing discrimination in medical settings can lead to decreased trust in health care systems, reduced satisfaction with health services, lower perceptions of the quality of care received, and negative relationships with health care teams. Discrimination also has the potential to affect an individual’s timeliness and adherence to treatment.
Community survey findings show an alarming 47 percent (N = 69) of South Ward residents reported having been unjustly prevented from accessing a service in the past year, or being treated unfairly by a service provider. While this question was not limited to health care services, it nonetheless speaks to the challenges (racial and otherwise) that a significant number of South Ward residents face, even when living in a predominantly Black community that includes Black health care and service providers.
During interviews, we asked South Ward residents and key stakeholders about the quality of health care services available in the South Ward. Both groups reported instances of racist, unfair, and inappropriate treatment by medical professionals due to race, age, appearance, and languages spoken. When asked specifically about their experiences of health care-related racism, one caregiver shared the following:
“I prefer not to have a White doctor. I also prefer a female doctor, but I let my children decide if they are comfortable. I do not prefer a White doctor because I have had some bad experiences, especially with them not believing me when I tell them I am in pain.”
A stakeholder interviewed for this study spoke about witnessing and reporting improper behavior by a physician toward an adolescent pregnant person because of her age and the fact that she had terminated previous pregnancies. The stakeholder noted that not only was the doctor’s behavior and line of questioning condemnatory, the doctor was also a “woman of color,” which—from the stakeholder’s perspective—made the situation even more unsettling. We also heard from a South Ward resident who had experienced racist and discriminatory treatment within predominantly Black health care systems. These experiences are not unique and align with other research suggesting that minoritized and marginalized people take on the characteristics of the dominant population and can engage in racist behaviors.[iii]
Another caregiver shared their experience of waiting for services in a medical facility and feeling as if they were being judged and made to feel “dirty” because of their appearance and clothing. This individual stated:
“… I try to avoid the hospital as much as I can because I feel like people make assumptions about me and are judging me.”
In addition to one’s demographic characteristics, respondents reported that the type of health insurance coverage an individual had also played a role in residents’ perceptions of the quality of health care they received. This is a significant issue, as almost half of South Ward residents (47%) rely on Medicaid as a primary source of health insurance (see Table 1). One resident reported the following:
“… The services [with Medicaid coverage] look a lot different than private insurance … I’m gonna give you two scenarios because I’m a mom who has private insurance. I walk in. The doctor gives me a little bit more time to discuss my issues …They’ll provide me with other information, you know, milestones, where my child should be. OK, you have someone who has Medicaid. They come in and it’s the basic, we’ll weigh the child, we’ll discuss if there’s any issues, and we’ll provide vaccines.”
In interviews, caregivers and stakeholders also discussed challenges of patients not feeling heard, health care providers not taking the time to listen to patients’ needs or concerns, and an overall lack of trust in medical providers. One caregiver said:
“The pediatrician I used for over two years, she doesn’t really take time to look at the child. I just need someone that’s willing to listen to me, understand, understand my children. Because all children are different …”
Several caregivers anticipate that the South Ward Wellness Center will fill a health care void.
FQHCs provide essential preventive and primary health care services to communities that have limited resources and can reduce health care obstacles such as a lack of insurance, transportation, and communication barriers. FQHCs can also improve a patient’s prenatal experiences via the provision of comprehensive care that is patient-centered, convenient, and coordinated with other essential social services. One study found that pregnant women served at FQHCs had higher levels of adherence to recommended prenatal care than women who were served at a hospital. Another study found that race and class disparities in postpartum care attendance were eliminated when prenatal care was received in FQHCs.
The South Ward Wellness Center
The South Ward Wellness Center (the Center) is part of an emerging effort in the SWPN to move the initiative’s focus from crisis intervention and helping families survive, to the provision of health care and other supports and resources that support families to help them thrive. While the Center is still in its infancy, once it is fully operational (in approximately two years), it will be a family-focused one-stop-shop co-located in the SWPN space. This shared housing will allow coordination between PN staff and St. James Health case managers. As an FQHC, Center operations will also be informed by a community board.
Given the ongoing health care challenges and needs identified during the SWPN implementation process, helping pregnant people and parents access consistent care is an important goal for the SWPN. The SWPN is working on addressing this goal in partnership with St. James Health. This recent and evolving collaboration is in the early stages of assessing and responding to residents’ health care needs through the newly formed South Ward Wellness Center, an FQHC.
To begin to understand community perceptions, we asked interviewees about the Center in advance of its April 2022 launch. One caregiver shared their excitement about the launch:
“It would be so helpful to women my age. There is nothing like that for us right now and we are all very stressed. Stress with finding a job, or with the kids, [or] being back and forth from work.”
A stakeholder echoed this excitement:
“… I think many people, especially single mothers, will engage with the health center. There are a lot of benefits.”
Importantly, one of the Center’s aims is to support families’ enrollment in, and maintenance of, health insurance, a barrier highlighted by a South Ward caregiver:
“I have struggled with trying to get insurance for myself because of some errors in the paperwork. The children have always had insurance but there was some time that I did not.”
While the Center is still in the initial stages of implementation, interviewees offered recommendations about its operations. These included improving community outreach, addressing discriminatory practices that have resulted in negative opinions about Newark-based community health centers, and building trust with residents. A stakeholder shared:
“I know two FQHCs that have struggled to keep patients. I think it is important to build trust with families. That will make them feel comfortable to use the health center.”
Early Lessons Learned and Recommendations
The following early lessons learned and recommendations are informed by the SWPN evaluation, SWPN staff experiences, South Ward Wellness Center implementation experiences, and survey and interview data collected as part of this research study. They have been co-developed by Child Trends and SWPN staff and are designed to inform the efforts of local policymakers, health care and public health practitioners, and community organizations interested in supporting the physical and mental health care needs of South Ward residents. When considering these recommendations and lessons learned, it is important to recognize that full implementation of community-based initiatives and interventions takes time. As such, we expect these learnings and recommendations to evolve and expand as the SWPN and the Center become more established and grounded in the community.
Although they are specifically informed by findings from the South Ward, our recommendations may be applicable to other communities with similar populations that are experiencing comparable health-related challenges and/or implementing PN grants. Based on the data and analyses conducted for this brief, we have identified three primary recommendations: Use SWPN infrastructure to facilitate residents’ health care access; seek (and use) community engagement and feedback to inform health care provision; and participate in professional development and ongoing learning.
Use SWPN and community infrastructure to facilitate health care access.
Opening a wellness center in the South Ward may reduce some of the health care access barriers identified as part of this research study—including a lack of community-based health care facilities, minimal available appointments, the need to travel long distances for care, and the lack of anti-racist and/or discriminatory service provision.
During this early implementation stage of the South Ward Wellness Center, the Center should draw on the SWPN’s current successes and strengths to address and meet the basic needs of South Ward residents, thereby improving the SDoH and facilitating health care access. The SWPN initiative currently connects South Ward residents to person-centered supports through coordinated navigation services provided by a team of social workers called domain specialists and community health workers (CHWs), who are peer leaders and allies in the South Ward community. Domain specialists and CHWs are a key strength of the SWPN initiative’s efforts to deliver person-centered services; they also address SDoH, which are essential to supporting residents’ physical and mental health and well-being. As the Center becomes more firmly established in the South Ward community, and co-location with the SWPN occurs, coordination between the Center’s staff and the domain specialists and CHWs can help ensure that the Center’s patients have access to similar levels and types of supports provided to the SWPN’s families.
In addition to already existing Medicaid application assistance, consider hiring additional case managers or social workers at the Center to help with referrals to other resources that support SDoH. These could include housing, early care and education supports, and linkages to programs such as the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), which provides food and nutrition resources to families with infants and young children. The SWPN initiative has prior experience recruiting, hiring, and training staff (i.e., domain specialists) with these skills and capabilities, and can serve as a knowledgeable resource for the Center as its programming and services continue to get underway.
Seek community engagement and feedback to inform provision of respectful, culturally responsive care.
The history of medical exploitation against Black people in the United States, and the racist and discriminatory practices identified by South Ward residents when recounting their health care-related experiences, warrants immediate and ongoing attention. It will be critical for the SWPN and St. James Health to continue to solicit input and listen to the needs of residents to ensure that the Center is not just accessible to residents, but that it provides high-quality, culturally respectful care that is anti-racist, non-discriminatory, and addresses the South Ward community’s identified needs. Lessons from this study suggest it will be important to:
Use the Center as a vehicle to develop and implement a process for collecting feedback from residents. Ongoing feedback from intervention recipients and key stakeholders is a critical component of successful intervention implementation. In early stages of implementation, creating feedback loops and “improvement cycles” can facilitate successful intervention and initiative implementation. Feedback from South Ward residents, SWPN partner agency staff, and other social service providers in the area will be key for the Center to ensure that it provides high-quality, respectful, and person-centered services and care that address the needs of South Ward residents. FQHCs, including the Center, are required to establish a governing board on which over half of the members are patients served by the health center; the remaining members must represent the community where the health center is located, in terms of their demographic characteristics like race, ethnicity, and gender. As the SWPN revives its previously existing Community Advisory Board and the Center develops its Board in accordance with FQHC standards, we recommend that the Center develop a systematic process for collecting feedback from the SWPN and the Center’s Boards and patients about their experiences. Strategies should include solicitation of ideas for program improvement after each visit and the use of these data to make regular updates to strengthen the Center’s processes, staffing, policies, and service delivery. Activities like these have the potential to ensure that patients’ input is heard and incorporated into the Center’s operations.
Seek community input on other types of care that may be needed at the Center. While the Center will increase access to health care overall in the South Ward, gathering input from residents about the types of care they want to see at the Center can help ensure a greater match between residents’ specific needs and what the Center offers. For instance, early feedback has suggested a preference among pregnant people and women for the Center to be staffed with female obstetricians/gynecologists.[iv] To learn more about the type of care that South Ward residents desire, the SWPN and St. James Health can build from their current engagement with birthing people who participate in the South Ward Healthy Beginnings program.[12] They should also consider conducting landscape and community strengths and needs assessments as tools to identify needs while minimizing effort duplication and better aligning existing services.
Set up systems of accountability that integrate patient feedback and outcomes data. Team conversations about feedback related to the Center will be critical to providing respectful, culturally responsive care. Interviews, focus groups, and the aforementioned needs assessments with St. James Health are all potential ways to hear directly from residents about what culturally responsive care means and how it is operationalized. In addition, ensuring that feedback is not just solicited—but used and reviewed regularly—will help inform Center practices and policies.
Participate in professional development and continuous learning.
Provide Center staff with ongoing training, professional development, and coaching to ensure that all staff and providers are delivering respectful, culturally sensitive, and person-centered care. South Ward residents have expressed dissatisfaction with the quality of some health care delivered in the South Ward, which has included racist and discriminatory treatment from health care providers. Addressing these issues may help establish trust in the community and ensure that South Ward residents who elect to use the Center consistently receive high-quality and respectful care. Drawing on already existing resources that highlight the ways in which systemic, interpersonal, and internalized racism and implicit biases play out in health care settings is an important first step for better serving residents. In addition, ongoing training and professional development that includes ways to reflect on, intervene, and stop harmful behaviors may prove to be an effective strategy to achieving higher-quality health care in the South Ward.
Conclusion
This brief has examined health care-related challenges experienced by residents in the South Ward community of Newark, NJ. These challenges include a lack of access to primary care providers, barriers to accessing care related to SDoH, and racist and discriminatory practices that affect the quality of care residents receive. In response to these issues, we drew on the recommendations of those who participated in the data collection processes for this brief, as well as our own experience in the SWPN, to provide concrete action steps for the South Ward Wellness Center to support higher-quality health care for South Ward residents. As the Center continues its expansion, we invite readers to access the SWPN website to learn more about the Center’s soft opening (underway since April 2022) and its official launch (projected for Fall 2024).
Acknowledgements
Our team is grateful to Dominique Lee (founder and CEO of the SWPN), Nichelle Holder (chief program officer for the SWPN), and Justine Asante (director of partner operations for the SWPN) for their partnership, collaboration, and commitment to ensuring the SWPN is working toward meeting the needs of community residents. We also appreciate our Child Trends colleagues—Kelley Bennett, Porsche Boddicker-Young, Brent Franklin, Maggie Haas, Elizabeth Jordan, Olga Morales, Catherine Nichols, Melissa Perez, Katelyn Rust, Jessica Warren, Andra L. Wilkinson, Renee Ryberg, James Fuller, Claire Kelley, and Maeve Day—who helped to strengthen this brief via the provision of constructive feedback and editorial and design assistance.
About this series
This brief is part of a larger effort by Child Trends researchers to expand knowledge about Black children and families. This effort includes an exploration of Black family cultural assets and the development of a multi-year applied research agenda on Black children and families. While these publications sometimes prioritize adults within Black families and sometimes prioritize children, the goals of the publications and research agenda are consistent—to build a deeper understanding of the diversity of Black families, contextualize their experiences within systems and institutions, and produce evidence to inform policies and practices that promote their well-being in the twenty-first century.
Footnotes
[1] The Department of Education awarded the SWPN an additional $30 million Promise Neighborhood Grant in 2021.
[2] New York University conducted a needs and segmentation analysis in 2016 to inform the SWPN application process. Their analysis indicated that the Upper Clinton Hill and Dayton neighborhoods had concentrated needs, which informed the SWPN’s decision to focus its efforts in these two neighborhoods.
[3] FQHCs are community-based health centers located in previously underserved areas. FQHCs offer care using a sliding scale fee and their governing board must include patient representatives .
[4] MUAs are defined and designated by HRSA as census tracts with “too few primary care providers, high infant mortality, high poverty, and/or high elderly population.”
[5] Retail-based health care includes health centers located in retail locations like drugstores (e.g., Walgreens, CVS) or general merchandise retailers (e.g., Target, Walmart) that provide affordable care for minor health needs.
[6] These zip codes include areas outside of the catchment area because some families send their children to schools in the South Ward from surrounding areas.
[7] We were not able to randomly assign survey participants due to the pandemic, so the data included in Table 2 are not representative of the community.
[8] Urgent care facilities and retail-based health clinics were presented as one response option in our survey, although these two facility types provide different levels of service. Retail-based health clinics are typically used to address minor illness or injury or for preventative needs such as vaccinations or health screenings. Urgent care facilities also provide these services, but must have a board-certified doctor, a nurse practitioner, and physician assistant on staff, which enables them to treat more acute illnesses and injuries (e.g., broken bones, non-life-threatening asthma treatment).
[9] The Healthy People 2030 initiative defines SDoH as “the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.”
[10] NBIMC also highlighted challenges with long wait times and scheduling appointments in a 2019 survey of 466 residents in Newark and surrounding areas.
[11] A 2019 focus group held with local medical professionals at NMBIH revealed that undocumented immigrants were denied services for refusing to disclose their personal information (such as financial or immigration information) at school-based clinics—a practice that further limits the available health care options for immigrant populations in the South Ward and Newark.
[12] The South Ward Healthy Beginnings (SWHB) program works to strengthen the outcomes of families and children by providing family- and child-centered supports such as stress reduction, and by supporting children’s skill development and responsive relationships with adults and children.
References
[i] Cifuentes, F., & Sherrer El, K. (2019). Achieving health equity and increasing access to health services in the South Ward: Feedback from stakeholders of the South Ward Children’s Alliance. Internal document.
[ii] Jones, J. H. (1981). Bad blood: The Tuskegee syphilis experiment (1st ed.). Free Press.
[iii] Hardiman, R., Jackson, B., & Griffin, P. (2007). Conceptual foundations for social justice education. In M. Adams, L. A. Bell, & P. Griffin (Eds.), Teaching for diversity and social justice (pp. 35–66). Routledge/Taylor & Francis Group.
[iv] Child Trends & South Ward Promise Neighborhood staff, personal communication, August 8, 2022.
Suggested citation
Ekyalongo, Y. Y., Lloyd, C. M., Steber, K., Patel, A., & Rivera, J. (2022). Understanding health care access and needs for Black families with children. Child Trends. https://doi.org/10.56417/8772q2793c
© Copyright 2025 ChildTrendsPrivacy Statement
Newsletter SignupLinkedInYouTubeBlueskyInstagram


